Mental health care is undergoing a meaningful shift. While traditional psychiatry has long focused on medication and talk therapy, a growing body of research highlights the powerful connection between nutrition, brain chemistry, and emotional well-being. This emerging field—known as nutritional psychiatry—is reshaping how clinicians approach mood disorders such as depression, anxiety, and chronic stress.
For integrative medicine practices, functional health clinics, and mental wellness providers, nutritional psychiatry offers a more holistic, patient-centered framework. It recognizes that what patients eat—and how their bodies process nutrients—can significantly influence neurotransmitter balance, inflammation, and overall mental health.
In this article, we explore the role of nutritional psychiatry in mood disorders, why it’s gaining momentum, and how integrative clinics can support this approach within a structured, data-driven care model.
What Is Nutritional Psychiatry?
Nutritional psychiatry is a clinical approach that examines how diet, nutrient status, and metabolic health affect brain function and mental health outcomes.
Rather than treating mood disorders in isolation, nutritional psychiatry considers factors such as:
- Micronutrient deficiencies
- Gut health and the microbiome
- Blood sugar regulation
- Inflammation and oxidative stress
- Dietary patterns and food quality
This approach does not replace conventional mental health care—it complements it by addressing underlying physiological contributors that may influence mood, cognition, and emotional resilience.
The Gut-Brain Connection and Mental Health
One of the foundations of nutritional psychiatry is the gut-brain axis—a bidirectional communication network linking the gastrointestinal system and the central nervous system.
Research shows that:
- Gut bacteria play a role in neurotransmitter production
- Inflammation in the gut can influence mood regulation
- Poor gut health may exacerbate anxiety and depressive symptoms
By addressing nutrition and digestive health, clinicians can support healthier signaling between the gut and brain, creating a more stable foundation for emotional well-being.
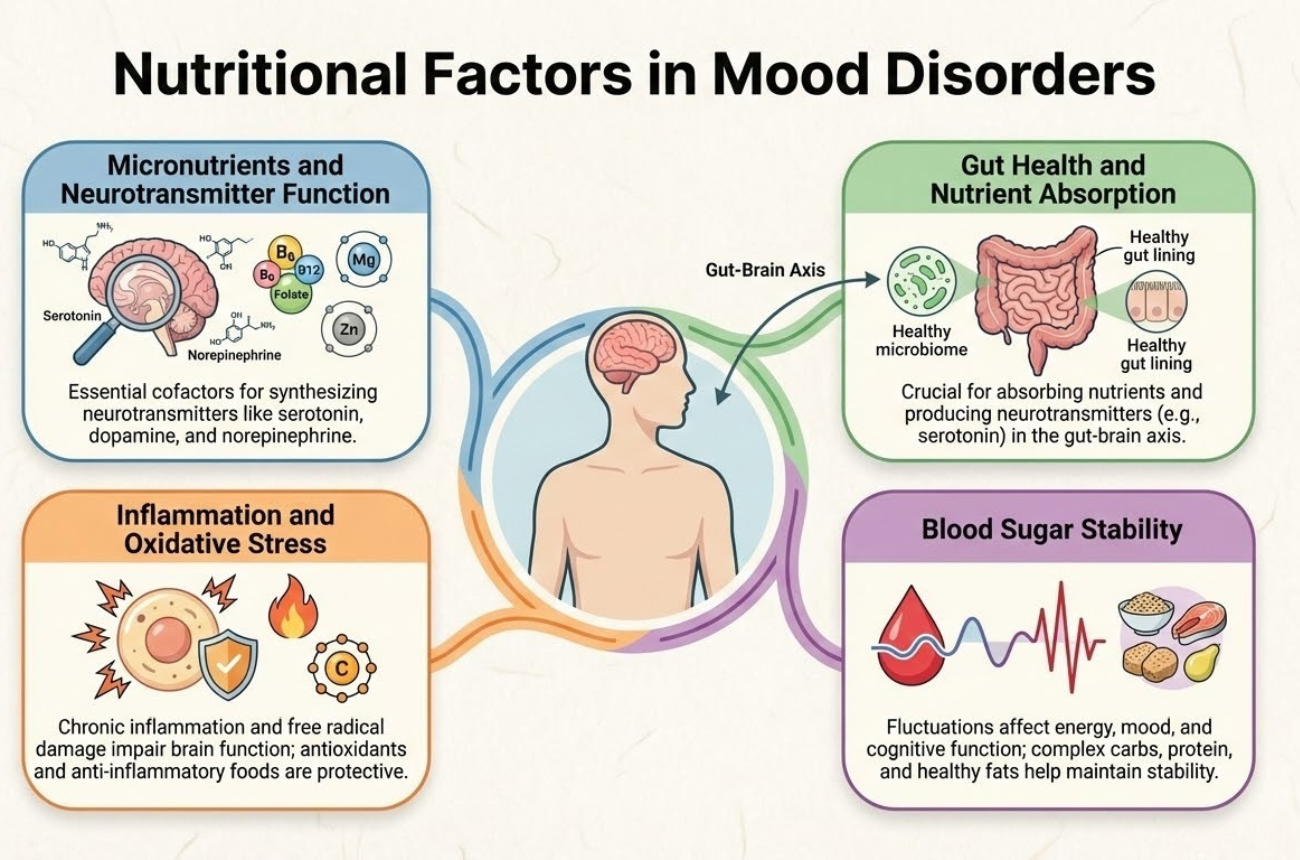
Key Nutritional Factors in Mood Disorders
While mood disorders are complex and multifactorial, nutritional psychiatry research consistently highlights several nutritional factors that play a meaningful role in emotional regulation, cognitive function, and mental resilience. These factors do not act in isolation; instead, they interact with neurochemistry, hormones, inflammation, and metabolic health to influence mood over time.
Understanding and assessing these nutritional elements allows clinicians to identify potential contributors to symptoms and design more personalized, supportive care plans.
Micronutrients and Neurotransmitter Function
Micronutrients are foundational to brain chemistry. Nutrients such as magnesium, zinc, B vitamins (particularly B6, B9, and B12), iron, and omega-3 fatty acids are directly involved in neurotransmitter synthesis, nerve signaling, and neuronal protection.
When these nutrients are deficient or poorly absorbed, patients may experience symptoms commonly associated with mood disorders, including:
- Persistent fatigue or low energy
- Irritability or emotional reactivity
- Depressed mood or apathy
- Brain fog, poor focus, or memory challenges
Nutritional psychiatry emphasizes identifying and addressing these deficiencies through diet, targeted supplementation when appropriate, and ongoing monitoring to support neurological balance.
Blood Sugar Stability
Blood sugar fluctuations can have a significant impact on mood, anxiety levels, and cognitive clarity. Rapid spikes and crashes in glucose levels may contribute to irritability, nervousness, fatigue, and difficulty concentrating—symptoms that can overlap with or worsen mood disorders.
From a nutritional psychiatry perspective, supporting blood sugar stability involves:
- Encouraging balanced meals with adequate protein, fiber, and healthy fats
- Reducing reliance on highly refined carbohydrates and sugars
- Promoting consistent meal timing to avoid prolonged fasting or crashes
Stable blood sugar supports more consistent energy levels and helps regulate stress hormones that influence emotional responses.
Inflammation and Oxidative Stress
A growing body of research links chronic, low-grade inflammation to depression, anxiety, and other mood disorders. Inflammatory processes can affect neurotransmitter metabolism, disrupt neural signaling, and influence the stress response system.
Dietary patterns rich in whole foods—such as vegetables, fruits, healthy fats, and anti-inflammatory nutrients—may help reduce inflammatory markers and oxidative stress. Nutritional psychiatry often focuses on:
- Increasing antioxidant intake
- Supporting healthy fat balance
- Reducing inflammatory dietary triggers
By addressing inflammation, clinicians can help create a physiological environment more conducive to emotional stability and recovery.
Gut Health and Nutrient Absorption
Even when diets appear adequate, gut health plays a critical role in whether nutrients are properly absorbed and utilized. Digestive imbalances, altered microbiome composition, or intestinal inflammation can interfere with nutrient availability and neurotransmitter production.
Supporting gut health is therefore a key component of nutritional psychiatry, as it directly influences how effectively nutritional interventions translate into mental health benefits.
Nutritional Psychiatry in Clinical Practice
Integrating nutritional psychiatry into mental health care requires more than dietary advice—it calls for structured evaluation, monitoring, and personalization.
Clinics offering nutritional psychiatry often incorporate:
- Comprehensive patient assessments
- Dietary and lifestyle evaluations
- Lab testing to identify deficiencies or imbalances
- Personalized nutrition plans aligned with mental health goals
- Ongoing follow-up to track progress over time
This approach supports long-term outcomes by addressing root contributors rather than symptoms alone.
The Role of Integrative Care Models
Nutritional psychiatry naturally complements integrative and functional medicine, which view mental health as interconnected with physical, metabolic, and lifestyle factors. By addressing diet, gut health, inflammation, and stress alongside traditional care, clinicians can target underlying contributors to mood disorders rather than only managing symptoms.
When combined with therapy, medication management when appropriate, and lifestyle interventions, nutritional strategies allow clinics to deliver personalized, holistic care. This approach improves patient engagement, supports adherence, and promotes more sustainable improvements in mood and overall well-being.
How OptiMantra Supports Nutritional Psychiatry Workflows
As awareness grows around the connection between nutrition and mental health, nutritional psychiatry is poised to play an increasingly important role in mood disorder treatment. Patients are seeking care that looks beyond prescriptions alone—care that considers their biology, lifestyle, and long-term well-being.
Clinics that embrace this approach can deliver deeper, more sustainable outcomes, but doing so effectively requires organized, longitudinal documentation and seamless collaboration across care disciplines. This is where an EMR and practice management system like OptiMantra becomes essential.
OptiMantra is designed to support integrative mental health practices by enabling clinics to:
- Document nutrition-focused assessments and care plans
- Track mood-related outcomes alongside dietary interventions
- Integrate lab results, notes, and follow-ups in one chart
- Maintain clear, audit-ready records for holistic treatment plans
- Support multidisciplinary collaboration across providers
By centralizing clinical data, OptiMantra helps practices deliver thoughtful, personalized mental health care grounded in whole-person wellness. Try a free trial or schedule a live demo to see how OptiMantra can streamline your nutritional psychiatry workflow today!
Nutritional Psychiatry FAQs
What is nutritional psychiatry?
Nutritional psychiatry is a field that studies how diet, nutrients, and metabolic health influence brain function and mental health, particularly mood disorders.
How does nutrition affect mood disorders?
Nutrition impacts neurotransmitter production, inflammation, gut health, and blood sugar regulation—all of which play a role in mood and emotional stability.
Can nutritional psychiatry help with depression and anxiety?
Nutritional psychiatry may support depression and anxiety management by addressing nutrient deficiencies, improving gut health, and reducing inflammation as part of a comprehensive care plan.
What types of providers use nutritional psychiatry?
Integrative physicians, functional medicine practitioners, mental health providers, and wellness clinics commonly incorporate nutritional psychiatry into patient care.
How does OptiMantra support integrative mental health care?
OptiMantra supports integrative mental health care by enabling structured documentation, longitudinal tracking, and collaboration across nutrition, mental health, and medical disciplines.
Legal Disclaimer: This article is for informational purposes only and does not constitute medical, nutritional, or mental health advice. Nutritional interventions and mental health treatments should be personalized and overseen by qualified healthcare professionals. Always consult appropriate providers before making changes to treatment plans.




